Mechanisms of Probiotics in Blood Sugar Control
Probiotics, found in foods like yogurt and supplements, may help manage blood sugar by improving gut health. Research shows they can slightly lower HbA1c (by 0.33% to 0.48%) and improve insulin resistance. They work by:
- Boosting short-chain fatty acids (SCFAs) that improve glucose metabolism.
- Strengthening the gut lining to reduce inflammation.
- Influencing hormones like GLP-1, which regulate insulin and appetite.
Probiotics are most effective when combined with a balanced diet, exercise, and prescribed treatments. Choose products with specific strains (Lactobacillus, Bifidobacterium) and consult your doctor before use.
How Probiotics Affect Blood Sugar Regulation
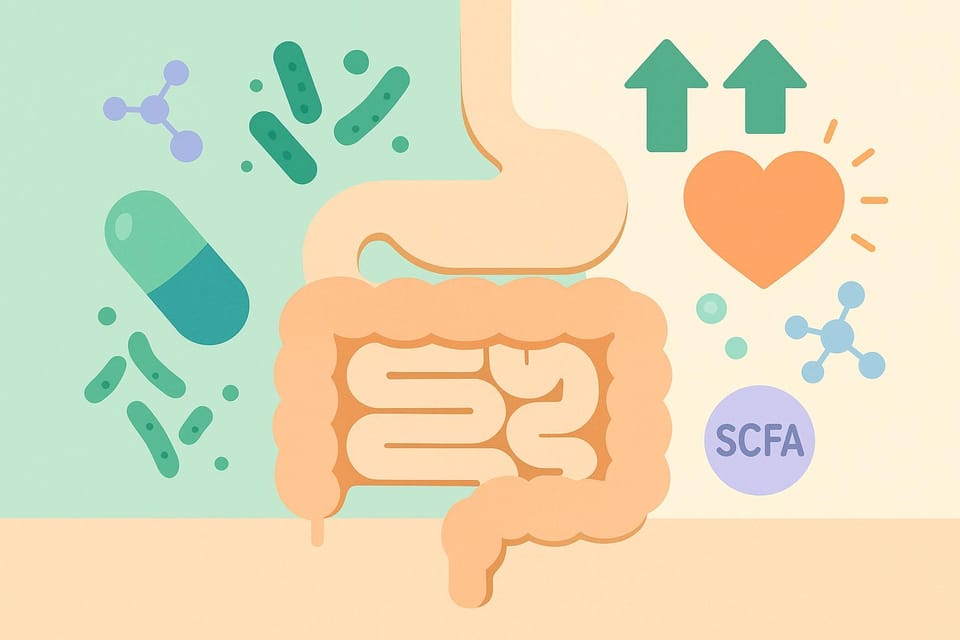
How Probiotics Regulate Blood Sugar: 3 Key Mechanisms
Probiotics play a role in blood sugar management through several complex biological processes. By reshaping the gut microbiome, they encourage metabolic changes that improve insulin sensitivity and help regulate glucose levels. Below, we’ll dive into the key mechanisms that make this possible.
Gut Bacteria Changes and SCFA Production
Probiotic strains like Lactobacillus and Bifidobacterium shift the balance of gut bacteria, increasing the presence of beneficial microbes while reducing harmful ones that produce lipopolysaccharides (LPS). This shift boosts the fermentation of dietary fiber into short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate. These SCFAs strengthen the gut lining, influence liver glucose production, enhance satiety, and regulate glucose and fat metabolism.
SCFAs also activate receptors (GPR41 and GPR43), which improve insulin sensitivity. Clinical studies show that increased SCFA production can lower HbA1c levels by 0.3 to 0.4 percentage points and improve insulin resistance metrics, especially when probiotics are combined with a fiber-rich diet. Additionally, SCFAs help reinforce the intestinal barrier, reducing inflammation by preventing endotoxins like LPS from leaking into the bloodstream.
Stronger Gut Barrier and Lower Inflammation
Probiotics enhance the gut’s protective barrier by increasing the production of tight junction proteins, such as occludin and claudins, and thickening the mucus layer. This helps prevent bacterial endotoxins from entering the bloodstream, reducing metabolic endotoxemia and the chronic low-grade inflammation that can interfere with insulin signaling.
Meta-analyses of adults with type 2 diabetes have shown that probiotics can lower inflammation and improve insulin resistance. For example, a review of eight randomized controlled trials found that probiotic interventions lasting 6 to 24 weeks resulted in a significant reduction in HOMA-IR scores (standardized mean difference of -1.36; 95% CI -2.30 to -0.41, p=0.005).
Hormone Effects on Glucose Balance
Probiotics and their SCFA byproducts also influence hormones that regulate blood sugar. SCFAs stimulate L-cells in the intestines to release incretin hormones like GLP-1 and PYY. GLP-1 enhances insulin secretion after meals, reduces glucagon release, slows gastric emptying, and promotes feelings of fullness. PYY complements this by further slowing gastric emptying and suppressing appetite. Together, these hormonal effects help smooth out post-meal blood sugar spikes, though they are less pronounced than those achieved with prescription GLP-1 medications.
Probiotics also impact bile acid metabolism through bile salt hydrolase activity, which can further improve glucose and fat regulation. Meta-analyses of prediabetic adults have observed reductions in both HbA1c and HOMA-IR, partially due to these hormonal changes.
| Mechanism | Key Process | Impact on Blood Sugar |
|---|---|---|
| Gut Bacteria & SCFA | Enhanced microbial diversity and SCFA production | Improved insulin sensitivity |
| Gut Barrier & Inflammation | Strengthened gut lining and reduced LPS leakage | Better insulin signaling and lower HbA1c |
| Hormones | Increased GLP-1 and PYY secretion, altered bile acid metabolism | Enhanced insulin release and glucose balance |
These processes take time, typically weeks to months, to show measurable benefits. When paired with a balanced diet, regular exercise, and prescribed medications, probiotics can be a helpful addition to blood sugar management. For guidance on choosing high-quality, research-backed probiotic products, tools like SlipsHQ can help ensure you’re making informed decisions.
What the Research Shows
Effects on Fasting Glucose, HbA1c, and Insulin Resistance
Research continues to shed light on how probiotics can positively impact key blood sugar markers in individuals with prediabetes and type 2 diabetes. Several meta-analyses highlight that probiotic supplementation reduces HbA1c levels by 0.33% to 0.44% and significantly lowers HOMA-IR, a key measure of insulin resistance. These effects tend to be most noticeable after 6 to 8 weeks of consistent use.
However, findings on fasting glucose levels vary. While one meta-analysis of 16 trials reported significant reductions in fasting plasma glucose, other studies observed trends toward improvement without reaching statistical significance. In a specific trial involving patients with diabetic nephropathy, 12 weeks of probiotic use led to a drop in fasting blood glucose from 10.68 mmol/L to 7.81 mmol/L and a reduction in HbA1c from 8.19% to 6.92% (p<0.05). The placebo group, in contrast, showed no changes. Additionally, fasting insulin levels consistently decreased across several studies. These findings underscore the potential of probiotics to improve metabolic markers, especially when considering specific strains and treatment durations.
The improvements in insulin resistance are particularly compelling. Probiotics appear to work by stimulating GLP-1 secretion, reducing inflammatory markers like IL-6 and TNF-α, and increasing the production of short-chain fatty acids. Notably, their impact tends to be greater on post-meal glucose levels than on fasting levels.
Differences Between Strains and Treatment Duration
The type of probiotic strain and the length of treatment play a crucial role in determining outcomes. Lactobacillus and Bifidobacterium species consistently show the strongest benefits across studies. For example, a six-month trial using the Lab4P probiotic blend demonstrated sustained improvements in obese individuals. Participants experienced an increase in beneficial gut bacteria, a reduction in harmful bacteria, and a decrease in overall blood sugar levels. These strains are known to enhance GLP-1 release, support pancreatic β-cell function, and improve gut flora balance, all of which contribute to reduced insulin resistance.
Treatment duration also matters. Short-term use (6 to 8 weeks) is effective in lowering HbA1c, fasting insulin, and HOMA-IR in people with type 2 diabetes. Longer interventions, ranging from 12 to 24 weeks, tend to deliver more sustained benefits. Most studies use daily doses of 10⁹ to 10¹⁰ CFU (colony-forming units) in multi-strain formulations, though specific dosages vary depending on the strain and study design.
While the results are promising, certain limitations remain. Studies often show moderate variability, small sample sizes, and inconsistent effects on body weight and fasting glucose levels. To address these gaps, experts call for larger, high-quality randomized controlled trials to better understand the time-dependent effects and to pinpoint the most effective strains and dosages. For now, probiotics seem to provide added benefits to standard diabetes care. Tools like SlipsHQ can help you determine whether specific probiotic supplements include research-backed strains at effective doses.
How to Use Probiotics for Blood Sugar Management
Choosing the Right Probiotic Supplements
When selecting a probiotic, focus on the specific strains listed on the label. Look for names like Lactobacillus casei Shirota or Bifidobacterium lactis rather than vague terms like "Lactobacillus spp." This is important because the effects on blood sugar are strain-specific, and most clinical studies evaluate particular strains or combinations. Opt for products that clearly state the strain names and offer daily doses between 1 and 10 billion CFU, as these amounts are typically supported by research for managing prediabetes or type 2 diabetes. Keep in mind, more CFUs don’t always mean better results - it’s about matching the strains and doses used in studies.
Since probiotics are classified as dietary supplements in the U.S., their quality can vary widely. To identify reliable options, look for third-party testing seals and clear, detailed labeling. Tools like SlipsHQ can help you verify strain names, CFU counts, and safety information. This app also flags potential allergens, safety warnings, and manufacturing standards, making it easier to avoid low-quality or contaminated products. High-quality probiotics, when paired with proven lifestyle habits, can support blood sugar management more effectively.
Safety and Precautions
Once you’ve chosen a probiotic, it’s important to consider safety and any potential limitations. For most adults, probiotics are safe and generally well tolerated, with temporary gastrointestinal discomfort being the most common side effect during the first few days. However, certain groups need to exercise caution. People with compromised immune systems - such as those undergoing chemotherapy, taking high-dose steroids, or living with advanced HIV - should use probiotics only under medical supervision, as there have been rare cases of bacteremia. Similarly, individuals with central venous catheters, severe critical illnesses, short bowel syndrome, severe pancreatitis, or significant cardiac valvular disease should consult a specialist before starting probiotics.
It’s also essential to talk to your healthcare provider, especially if you’re on medications like metformin or insulin. Establishing baseline glucose markers is a good idea, as research shows probiotics are more effective at improving HbA1c and insulin resistance than significantly lowering fasting glucose. Plan to monitor your progress - such as repeating HbA1c tests every three to six months and tracking home glucose readings - while maintaining a stable routine of diet, exercise, and medications.
What to Expect From Probiotics
Understanding the timeline for potential benefits is just as important as selecting the right product. Research suggests that probiotics can lead to modest but meaningful improvements when used consistently. For example, meta-analyses show they can reduce HbA1c by about 0.3 percentage points and improve insulin resistance (measured by HOMA-IR) in people with type 2 diabetes. However, changes in fasting blood glucose are usually smaller and less predictable. Most studies involve interventions lasting 6 to 24 weeks, with noticeable benefits often appearing after 6 to 8 weeks. So, you’ll need to use probiotics consistently for at least 2–3 months to see measurable results, alongside regular check-ins with your healthcare provider.
Probiotics work best as part of a broader strategy for managing blood sugar. Combine them with a high-fiber, plant-based diet, regular physical activity (like 150 minutes per week of moderate aerobic exercise), and any prescribed medications. They’re not a standalone solution but rather one piece of a larger puzzle that includes good sleep, stress management, and maintaining a healthy weight. Each of these factors adds up, helping you create a more effective approach to metabolic health.
Conclusion
Probiotics provide a steady and practical option to help manage blood sugar levels through various biological mechanisms. They can reshape gut microbiota, boost the production of short-chain fatty acids, strengthen the intestinal lining to reduce chronic inflammation, and influence hormones like GLP-1, which play a role in glucose regulation. Research, including meta-analyses, shows modest improvements in markers like HbA1c and insulin resistance, particularly in individuals with prediabetes. While changes in fasting blood sugar levels are often smaller and less consistent, the improvements in long-term markers like HbA1c suggest better overall glucose management.
That said, it’s essential to have realistic expectations. Probiotics require consistent use over weeks to show benefits and are not a quick solution or a substitute for core diabetes treatments. They work best as part of a comprehensive approach that includes a balanced diet, regular exercise, prescribed medications, and ongoing monitoring. Their effectiveness is maximized when used under the guidance of healthcare professionals.
Before starting probiotics, consult your doctor - especially if you’re using insulin or managing other serious health conditions. Your healthcare provider can help you establish baseline lab values and track any changes over time. Since the quality and composition of probiotic products can vary widely, tools like SlipsHQ can help verify that the strains and doses listed on the label match those used in research. They can also flag safety concerns, allergens, and pricing options to help you find a reliable product that fits your needs.
While the research is encouraging, larger studies are still needed to standardize probiotic therapies. Not all products will yield the same outcomes, so selecting research-backed strains and using them consistently is key. By working closely with your healthcare team, you can make informed choices that support your long-term metabolic health.
FAQs
How do probiotics help improve insulin sensitivity?
Probiotics can improve how the body responds to insulin by supporting a healthier gut microbiome. They encourage a balanced mix of gut bacteria, which is crucial for managing blood sugar levels. On top of that, probiotics help lower inflammation and reinforce the gut lining - both factors tied to better insulin function.
By aiding these processes, probiotics play a helpful role in maintaining steady blood sugar levels, making them a smart choice for anyone prioritizing metabolic health.
Which probiotic strains are most effective for supporting healthy blood sugar levels?
Certain probiotics, like Lactobacillus rhamnosus and Bifidobacterium longum, have been linked to better blood sugar regulation. These strains may help by promoting a healthier balance of gut bacteria - an essential factor in metabolic health - and by lowering inflammation that can disrupt glucose management.
While probiotics can contribute to overall health, it’s crucial to select supplements that contain these specific strains and are of high quality. Make sure to consult a healthcare provider to confirm they align with your individual health needs and goals.
How long does it take for probiotics to help with blood sugar control?
Most individuals might see changes in their blood sugar levels after 4 to 8 weeks of regularly taking probiotics. That said, the exact timeline can differ based on factors such as the probiotic strain, dosage, and personal health conditions.
To get the best results, opt for high-quality probiotics and stick to the suggested usage instructions. Staying consistent is crucial when adding probiotics to your daily routine.