Supplements During Pregnancy: Risks vs. Benefits

Pregnancy supplements can support your health and your baby’s development, but they’re not all created equal. Here's what you need to know:
- Key nutrients like folic acid, iron, iodine, vitamin D, and omega-3s are often necessary during pregnancy to meet increased nutritional needs.
- Misuse of supplements - like taking too much vitamin A or iron - can lead to harmful side effects, including birth defects and health complications.
- Regulation gaps in the U.S. mean some supplements may be mislabeled or contaminated. Always choose third-party-tested products.
- Consult a healthcare provider before starting any supplement to ensure proper dosage and avoid unsafe ingredients.
- Tools like SlipsHQ can help you verify supplement safety by scanning barcodes and reviewing detailed ingredient information.
Start with a high-quality prenatal vitamin, focus on a nutrient-rich diet, and avoid unregulated herbal or weight-loss supplements. Always discuss your choices with your OB-GYN to make safe, informed decisions.

Safe vs. Unsafe Pregnancy Supplements: Essential Nutrients and Dosages
How to Assess Supplements During Pregnancy
What to Look For
Before starting any supplement, think about whether it’s truly necessary for your specific needs. This means considering factors like your lab results, diet, existing health conditions, and the stage of your pregnancy. Research suggests that most women benefit from a standard prenatal vitamin combined with key nutrients like folic acid and iron, making additional supplements often unnecessary. Always check that the supplement is supported by solid human pregnancy data, such as clinical trials or systematic reviews. Many herbal or specialty supplements lack this level of research.
Pay close attention to dosage. For example, around 400 mcg of folic acid daily is recommended, but exceeding 1,000 mcg without medical advice should be avoided. Timing matters, too - starting folic acid before conception or in early pregnancy can reduce the risk of neural tube defects, while other supplements might be more beneficial later on. Lastly, consult your OB-GYN, midwife, or pharmacist to review potential interactions. Certain herbs, especially those affecting blood clotting, or other supplements might influence blood pressure, mood, or blood sugar levels.
Using SlipsHQ to Check Supplement Safety
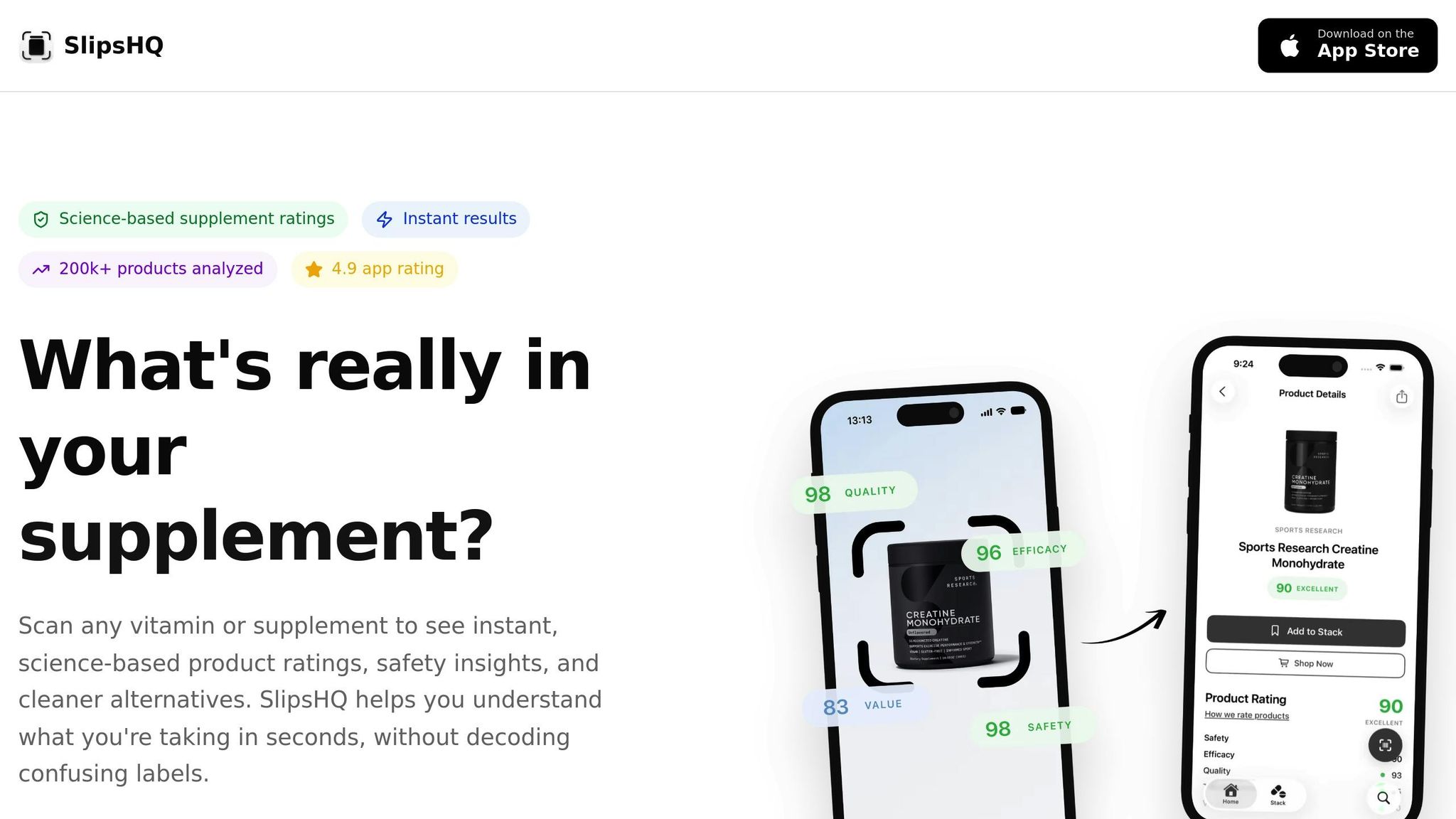
Once you know what to look for, digital tools can simplify the process. The SlipsHQ app lets you scan a product's barcode to access an independent profile with a full ingredient list, precise dosages, and pregnancy-related warnings. Its trust score (rated 0–100) evaluates factors like contaminant levels, label accuracy, and the strength of supporting evidence, giving you a quick snapshot of the product’s quality.
The app also flags ingredients that are often discouraged during pregnancy - like high doses of vitamin A, certain stimulants, or unverified herbal blends - and provides clear summaries of related research. Its personalized supplement stack feature is especially handy, helping you ensure that your prenatal vitamin and any additional products don’t push you over the recommended daily nutrient limits. You can even share the SlipsHQ report with your healthcare provider during prenatal visits for a thorough review.
Reading Labels and Following Guidelines
Even with digital tools, reviewing product labels yourself is essential. Start by comparing the "Amount per serving" to the serving size listed - taking multiple tablets or gummies could unintentionally increase your overall intake. Make sure dosages match the recommended daily allowances (RDAs) and stay within tolerable upper intake levels (ULs) for pregnancy. Add up nutrients from all sources, including prenatal vitamins, stand-alone supplements, and fortified foods, to avoid exceeding safe limits - especially for fat-soluble vitamins (A, D, E, and K) and minerals like iron.
Be cautious of red flags like megadoses of vitamin A, stimulant claims, proprietary blends that obscure dosages, or exaggerated health promises. Look for brands with third-party quality seals, such as NSF or USP, which verify that the product contains what it claims and is free from major contaminants. When in doubt, stick to the lowest effective dose that’s backed by evidence, rather than assuming that more is better.
Supplements That Help During Pregnancy
Folic Acid
Folic acid is a critical supplement for pregnancy, especially during the early stages. This synthetic form of folate supports essential fetal development. In the U.S., it’s recommended to take 400 mcg daily, starting at least one month before conception through the first trimester. For women at higher risk - such as those with a history of pregnancies affected by neural tube defects or those on certain anticonvulsants - doses may go up to 4 mg daily under medical supervision. However, the total intake from supplements and fortified foods should stay below 1,000 mcg (1 mg) per day to avoid potential complications.
Why is folic acid so important? It significantly lowers the risk of neural tube defects like spina bifida and anencephaly, which can develop before many women even realize they’re pregnant. Some studies also suggest that folic acid might help reduce risks of preeclampsia, preterm delivery, and low birth weight, though findings vary.
Since many grains in the U.S. are fortified with folic acid, it’s a good idea to review your overall intake with your healthcare provider to ensure you’re meeting - but not exceeding - the recommended levels.
Now, let’s look at iron, another key nutrient during pregnancy.
Iron
During pregnancy, your body’s need for iron increases from 18 mg to 27 mg daily to support the growing blood supply and your baby’s development. Iron is essential for producing hemoglobin, the protein in red blood cells that carries oxygen. Adequate iron intake helps reduce the risk of maternal anemia, fatigue, preterm birth, and low birth weight.
Most prenatal vitamins in the U.S. include 27 mg of elemental iron, but some women may need higher doses depending on bloodwork. For example, you might require more iron if you have pre-existing anemia, experience heavy menstrual bleeding, follow a vegetarian or vegan diet, or are carrying multiples. However, iron supplements can sometimes cause side effects like constipation, nausea, and dark stools. To ease these issues, try taking iron with food, at bedtime, or in a slow-release form. Increasing your fiber and fluid intake can also help. Be cautious about taking iron with calcium-rich foods or supplements, as calcium can interfere with absorption.
Always consult your healthcare provider to determine the right dosage based on your lab results and individual needs.
Beyond folic acid and iron, omega-3 fatty acids are another essential nutrient during pregnancy.
Omega-3 Fatty Acids (DHA/EPA)
Omega-3 fatty acids, particularly DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid), are vital for your baby’s brain and eye development. Adequate DHA levels in the mother have been linked to improved visual and cognitive outcomes in infants. Experts suggest 200–300 mg of DHA daily during pregnancy, which can be achieved by eating low-mercury fatty fish like salmon or sardines (about two servings per week) or by taking purified fish-oil or algae-based supplements.
When choosing an omega-3 supplement, look for products that clearly list DHA and EPA content, use purified sources (fish or algae), and meet third-party testing standards. Avoid supplements with unnecessary additives like herbal stimulants or high levels of vitamin A from fish liver oils. Since dietary supplements in the U.S. aren’t strictly regulated, opting for brands with third-party certifications can help ensure quality.
For those who are vegan, vegetarian, or don’t consume fish, algae-based DHA supplements offer a reliable plant-based option. Sharing your supplement choices with your healthcare provider during prenatal visits can help ensure they align with your overall nutrition plan.
Supplements to Avoid or Use Carefully During Pregnancy
High Doses of Fat-Soluble Vitamins
When it comes to fat-soluble vitamins during pregnancy, vitamin A raises the most concern. Excessive amounts of preformed vitamin A (like retinol and retinyl esters) can build up in the liver and fat, leading to serious birth defects. Experts in the U.S. recommend pregnant women limit their total vitamin A intake to below 10,000 IU (3,000 mcg RAE) daily from all sources. Most prenatal vitamins already include a safe amount, so it's best to avoid additional vitamin A supplements marketed for skin, anti-aging, or immune support. Instead, focus on getting vitamin A from beta-carotene found in fruits and vegetables, which your body converts safely as needed.
As for vitamin E, it's generally safe at prenatal levels, but doses exceeding 300 mg/day could interfere with blood clotting. Unless your healthcare provider advises otherwise, stick to the vitamin E provided in your prenatal vitamins. Vitamin D, another fat-soluble vitamin, is typically safe in amounts between 1,000–4,000 IU/day, but always follow your provider's guidance. It's also important to avoid combining multiple supplements containing vitamins A, D, or E, as fat-soluble vitamins can accumulate in the body and increase health risks. Always check product labels to avoid unintentional stacking.
Next, let’s look at stimulants and weight-loss products, which pose additional risks during pregnancy.
Stimulants and Weight Loss Products
Supplements like energy drinks, pre-workout formulas, and weight-loss products often contain high doses of caffeine, synephrine (bitter orange), yohimbine, or other thermogenic ingredients that can be dangerous during pregnancy. These compounds can elevate heart rate and blood pressure, and consuming more than 200 mg of caffeine daily has been linked to a higher risk of miscarriage. A single serving of a pre-workout supplement can pack 100–300 mg of caffeine, not to mention hidden sources like guarana or green tea extract that add even more caffeine.
Some weight-loss and mental-focus supplements also include vinpocetine, an ingredient flagged as unsafe for pregnancy due to potential risks to fetal development. Many of these products have not been tested on pregnant women, meaning their full risks are unknown. If you're already drinking coffee or tea, adding a stimulant supplement could easily push you over safe caffeine limits. The safest choice? Skip energy boosters, fat-burning supplements, and detox products altogether. Instead, focus on natural ways to stay energized, like getting enough sleep, staying hydrated, and maintaining a balanced diet.
Low-Quality or Unregulated Products
Quality control is another critical factor when choosing supplements during pregnancy. In the U.S., supplements are not FDA-approved, which means their quality can vary significantly. Low-quality products may be contaminated with heavy metals, pesticides, or bacteria, and inaccurate labeling could lead to overdosing or nutrient deficiencies. Even small errors - like too much vitamin A or iodine - can harm fetal development.
To reduce risks, look for supplements with third-party testing certifications from independent organizations, which verify purity and potency. Tools like SlipsHQ can help by scanning a supplement's barcode to display science-backed safety scores, ingredient details, and warnings about high-risk additives like excessive vitamin A or multiple stimulants. This app evaluates products based on Safety, Quality, and Transparency, making it easier to compare brands and steer clear of those with questionable practices. During pregnancy, choosing a reputable, thoroughly tested supplement is key, as even minor quality issues can have serious consequences.
Choosing Supplements Based on Your Needs
Common Situations That Affect Supplement Needs
When it comes to supplements, your diet and health history play a big role in determining what you might need to add. For instance, vegetarians and vegans often find it challenging to get enough vitamin B12, iron, iodine, and DHA from plant-based foods, so supplements can help fill those gaps. Similarly, women who avoid dairy might need extra calcium and vitamin D, either through supplements or fortified foods. If you’re dealing with iron-deficiency anemia, your doctor may recommend higher doses of iron than what’s in a standard prenatal vitamin. This usually involves follow-up blood tests to monitor hemoglobin and ferritin levels, while also managing potential side effects like constipation.
For women with thyroid conditions such as hypothyroidism or Hashimoto’s disease, iodine and selenium needs can be different. However, adding iodine on your own isn’t safe - too much or too little can negatively impact fetal thyroid development. If you have gestational diabetes, your care team might suggest adjustments to your vitamin D or magnesium intake. Additionally, if you’ve experienced preeclampsia, preterm birth, or had a baby with low birth weight in a previous pregnancy, your provider may focus on optimizing nutrients like folate and vitamin D, as studies link adequate supplementation to improved outcomes in these high-risk cases.
These factors are key when determining which supplements are right for you.
Steps for Making Safer Choices
Before adding new supplements to your routine, it’s crucial to consult your OB-GYN or midwife and share a full list of what you’re already taking. Start with a high-quality prenatal vitamin that includes 400–800 mcg of folic acid, 27 mg of iron, and recommended levels of iodine and vitamin D. Be sure to check labels for excessive fat-soluble vitamins and look for third-party testing certifications like USP or NSF.
A helpful tool like SlipsHQ can make the process easier by comparing safety scores and identifying risky additives. This app evaluates supplements based on Safety, Quality, and Transparency, helping you choose brands that align with your needs. Its personalized stacks feature can organize your supplements, prevent overlaps (like taking too much iron or vitamin A), and create a clear list to review with your healthcare provider.
It’s also a good idea to reassess your supplement routine at key points - like the start of a new trimester, after lab results, or if you’re diagnosed with conditions like anemia or gestational diabetes. This ensures your regimen evolves alongside your health.
Combining Research With Personal Circumstances
A well-thought-out supplement plan balances scientific guidelines with your individual circumstances. Start by reviewing your diet to identify any gaps. For example, if you’re not eating enough leafy greens, meat, dairy, or fish, those might be areas to address. Compare your food intake to U.S. prenatal nutrition targets with the help of your clinician or dietitian. If your diet is generally balanced - featuring fortified grains, fruits, vegetables, dairy or fortified substitutes, and some seafood - a quality prenatal vitamin often covers the needs of low-risk pregnancies.
However, if lab work reveals deficiencies - like low ferritin, vitamin D, or vitamin B12 - your provider may recommend higher doses of specific nutrients. These adjustments are usually monitored through follow-up labs to avoid under- or over-supplementation.
Women with restricted diets, severe nausea (such as hyperemesis gravidarum), malabsorption issues, or those expecting multiples often require more tailored supplementation since food alone may not meet their increased nutritional demands. It’s important to document these decisions and revisit them at each prenatal appointment, as your needs can change throughout pregnancy.
Conclusion: Making Smart Supplement Choices for a Healthy Pregnancy
When it comes to choosing supplements during pregnancy, the key is finding the right balance between meeting your needs and ensuring safety. This starts with a nutritious diet and a high-quality prenatal vitamin tailored to your specific requirements, which is often sufficient for most low-risk pregnancies. Additional supplements should only be introduced if your healthcare provider identifies a specific deficiency or medical need, like extra iron for anemia or vitamin B12 for those following a vegan diet.
It's important to stay cautious about certain supplements. Excessive amounts of fat-soluble vitamins, particularly vitamin A, can negatively impact fetal development. Similarly, unregulated herbal products or weight-loss supplements may contain unsafe additives. Since quality and labeling can vary significantly, always verify the contents of any supplement before taking it.
Tools like SlipsHQ can be invaluable in this process. By scanning product barcodes, you can access safety warnings, detailed ingredient information, and science-backed trust scores. This helps you avoid risky additives and ensures you're selecting higher-quality options. The app also allows you to compare brands, check prices in USD, and create a personalized supplement plan to review with your OB-GYN or midwife. While not a substitute for professional advice, it’s a practical way to streamline your decision-making.
Before making any changes to your supplement routine, consult your OB-GYN. Review your complete list of supplements alongside lab results to confirm proper dosages and steer clear of products marketed for weight loss or energy. A simple checklist can guide your choices: Do you have a confirmed deficiency? Is there strong evidence supporting the supplement's benefits? Has the dose and product quality been verified? And, most importantly, has your clinician approved it?
Ultimately, your supplement plan should be safe, personalized, and well-informed. Meeting your nutritional needs while avoiding risky products is crucial. By relying on essential nutrients, trusted tools like SlipsHQ, and professional guidance, you can make smarter choices for a healthier pregnancy.
FAQs
What are the risks of taking unregulated supplements during pregnancy?
Taking supplements without proper regulation during pregnancy can be risky for both the mother and the baby. These products might include harmful substances, contaminants, or incorrect dosages that could result in serious issues like developmental problems, allergic reactions, or even toxicity.
Unlike prescription medications, the supplement industry doesn’t face the same strict regulations. Some products may not undergo thorough testing to confirm their safety or effectiveness. To protect yourself and your baby, always talk to your healthcare provider before adding any supplement to your routine during pregnancy. They can help ensure it's safe and fits your specific needs.
How can I make sure the supplements I take during pregnancy are safe and effective?
Choosing supplements during pregnancy is a big deal - not just for your health, but for your baby's growth too. It's crucial to ensure that the products you choose are safe and of high quality.
One handy tool to consider is SlipsHQ. This app lets you scan barcodes to check a supplement’s safety, ingredient purity, and credibility. It also flags any safety warnings and provides science-based information, giving you the confidence to make well-informed choices for you and your baby.
Why should you talk to your doctor before taking supplements during pregnancy?
Before adding any supplements to your routine during pregnancy, it’s crucial to talk with your doctor. They can help ensure that the supplements you take are safe and appropriate for your specific health needs. Some supplements might include ingredients that could pose risks to you or your baby, interact with medications, or even provide nutrients in amounts that exceed recommended levels.
Your doctor can help you navigate these choices, recommending options that promote a healthy pregnancy while steering clear of unnecessary risks.