Vitamin D: Why Results Vary by Population

Vitamin D plays a key role in bone health, muscle function, and immune regulation. But not everyone benefits equally from supplementation, and results vary widely due to factors like skin tone, location, lifestyle, weight, and genetics. Here’s what you need to know:
- Who Needs Vitamin D Supplements: People with darker skin, those living in northern regions, individuals with obesity, or those who spend most time indoors are more likely to be deficient.
- What Research Shows: Supplements help if you’re deficient, but they don’t improve outcomes like heart health or cancer prevention for people with adequate levels.
- Why Differences Exist: Darker skin reduces vitamin D production from sunlight. Obesity stores vitamin D in fat, lowering blood levels. Genetics also influence how your body processes it.
- How to Decide: A blood test can show if you’re deficient. If so, supplements can improve your health. If not, extra supplementation may not help.
If you’re unsure about your levels, talk to your doctor and consider factors like your skin tone, location, and lifestyle to decide if supplements are right for you.
How Vitamin D Deficiency Varies Across Different Groups
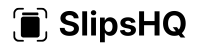
Vitamin D Deficiency Rates by Race and Ethnicity in the United States
Vitamin D deficiency doesn’t affect everyone in the U.S. equally. Between 2001 and 2004, only 23% of U.S. adolescents and adults reached levels of 30 ng/mL, leaving a striking 77% below the threshold for sufficiency. Even more concerning, the percentage of people with deficiency (below 20 ng/mL) rose from 22% to 36% between the late 1980s and early 2000s. However, these overall statistics hide significant variations tied to skin tone, geographic location, and lifestyle.
Differences by Race and Ethnicity
Vitamin D deficiency rates differ substantially across racial and ethnic groups. Non-Hispanic Black Americans experience the highest rates of deficiency, followed by Hispanic and some Asian populations, while non-Hispanic White adults tend to have the lowest rates. Data from NHANES (2001–2004) revealed that only 3% of non-Hispanic Black adults reached 30 ng/mL. More recent CDC data (2011–2014) showed that 17% of non-Hispanic Black adults had severe deficiency (below 12 ng/mL), compared to just 2% of non-Hispanic White adults.
The reason lies in melanin, the pigment responsible for skin color. Melanin absorbs UVB rays, which are crucial for converting 7-dehydrocholesterol in the skin into vitamin D₃. As a result, individuals with very dark skin may need 3–10 times more UVB exposure than those with very light skin to produce the same amount of vitamin D under identical conditions. For example, a Black office worker in Chicago faces far greater challenges in maintaining adequate vitamin D levels than a White landscaper in Phoenix, even before considering factors like time spent indoors or clothing choices.
Interestingly, despite lower vitamin D levels, Black Americans often exhibit better bone density and lower fracture risk compared to White Americans at the same vitamin D levels. This suggests that deficiency thresholds and associated health risks may not apply uniformly across all ethnic groups.
Effects of Location and Season
Your location within the U.S. plays a huge role in how much vitamin D your skin can produce. If you live above roughly 37°N latitude, your skin makes little to no vitamin D from November to early March. For instance, in Boston (42°N), no vitamin D production occurs between November and February, while Miami (25°N) allows for year-round production, though it still decreases during winter.
This results in a seasonal pattern: vitamin D levels tend to peak in late summer or early fall and then drop by 10–20 ng/mL by late winter or early spring, especially for those who reduce sun exposure during colder months. Given that vitamin D has a half-life of about 2–3 weeks, levels can decline noticeably over several months without supplementation. For example, someone in Minneapolis might have sufficient vitamin D in August but fall into deficiency by March without taking supplements.
Lifestyle and Body Factors
Daily habits and personal choices also influence vitamin D levels. Spending most of your time indoors or wearing long sleeves or head coverings can significantly reduce UVB exposure. Additionally, sunscreen with SPF 15 can block over 90% of vitamin D synthesis, although real-world application is often less thorough, so the actual reduction tends to be smaller. Other environmental factors, like air pollution or tall buildings in urban areas, further limit UVB rays from reaching the skin.
Age and body weight also play a role. Older adults produce less vitamin D because their skin contains lower levels of 7-dehydrocholesterol, and they may spend less time outdoors. Meanwhile, obesity (BMI ≥30) is consistently linked to lower circulating vitamin D levels. Since vitamin D is fat-soluble, it gets stored in fat tissue, leaving less available in the bloodstream. Studies show that people with obesity often have 20–30% lower vitamin D levels than those with a normal BMI. This means individuals with obesity typically require higher daily intakes of vitamin D to achieve the same blood levels as leaner individuals.
What Major Studies Show About Vitamin D Supplements
Research on vitamin D supplements highlights a clear pattern: the benefits largely depend on your starting vitamin D levels. If your levels are already sufficient, the gains are minimal. However, addressing a deficiency can lead to noticeable improvements.
Results in People with Normal Vitamin D Levels
Studies like the VITAL, ViDA, and DO-HEALTH trials have shown that taking 2,000 IU of vitamin D daily doesn’t significantly lower the risk of cardiovascular events, cancer, fractures, or falls in adults with normal vitamin D levels. For example, the VITAL trial reported a hazard ratio of 0.97 for cardiovascular events in this group. A 2021 review published in Nature Reviews Endocrinology summed it up well:
supplementation of vitamin D–replete individuals does not generate overall health benefits
Benefits for People with Deficiency or Higher Risk
The story changes for those who are deficient or at higher risk. Studies focusing on vitamin D–deficient, older, or frail populations - such as postmenopausal women - show that supplementation, often paired with calcium, can boost bone density and lower the risk of fractures.
Beyond bone health, there’s evidence that vitamin D can help prevent other conditions. The D2d trial found that in individuals with a deficiency, supplementation reduced the progression from prediabetes to type 2 diabetes. Two meta-analyses also reported about a 10% reduction in diabetes risk, particularly with doses over 1,000 IU/day and in people without obesity. Additionally, updated findings from the VITAL trial revealed a slight but meaningful reduction in cancer deaths - around a 13% decrease (hazard ratio of 0.87) - when participants took 2,000 IU/day. This suggests that vitamin D may help improve outcomes in older or higher-risk individuals once cancer has developed.
Why Different Groups Respond Differently to Vitamin D
The effectiveness of vitamin D isn't just about how much you take - it also depends on how your body produces, distributes, and processes it. These factors help explain why people respond differently to supplementation.
How Skin Color and Sun Exposure Affect Vitamin D
Melanin, the pigment responsible for skin color, plays a role in vitamin D production by acting like a natural sunscreen. It absorbs UVB rays in the skin, which reduces the amount of vitamin D your body can produce. This means that individuals with darker skin need 3–10 times more sun exposure compared to those with lighter skin to produce similar levels of vitamin D under the same conditions. Because of this, darker-skinned populations often have lower serum vitamin D levels. Living in northern areas, where the winter sun is too weak for effective vitamin D synthesis, further increases the risk of deficiency.
How Body Weight Affects Dosing Needs
Vitamin D is stored in fat, which means that in people with obesity, it tends to diffuse into fat tissue rather than circulating in the blood. Research from large trials shows that individuals with a body mass index (BMI) over 30 kg/m² experience smaller increases in blood vitamin D levels, even when taking the same dose as those with lower BMIs. This suggests that higher or longer-term supplementation may be necessary for these individuals to reach optimal levels.
Genetic Differences in Vitamin D Processing
Genetics also play a significant role in how the body processes vitamin D. Variations in certain genes, such as CYP2R1, CYP27B1, CYP24A1, and the GC gene (which affects the vitamin D binding protein), can influence how efficiently your body metabolizes and uses vitamin D. For example, some GC gene variants result in lower total vitamin D levels but maintain normal levels of "free" vitamin D, which is the active form. Findings from over 60 Mendelian randomization studies highlight how these genetic differences explain why some people see a quick rise in their blood levels with minimal supplementation, while others need higher doses to achieve similar results.
How to Apply This Research to Your Supplement Choices
Understanding Study Results for Your Situation
When considering how vitamin D research applies to you, it's important to dig deeper than the headlines. The details of a study - such as who participated and their circumstances - can make a big difference. For example, factors like age, race, ethnicity, geographic location, and sun exposure all influence how relevant the findings might be to your situation. If the study focused on older European women with severe vitamin D deficiency, the results may not translate to a young adult in Florida who already has sufficient levels.
Research consistently shows that people with adequate vitamin D levels (above 20 ng/mL) gain little from additional supplementation. On the other hand, studies targeting groups with clear deficiencies - such as individuals with darker skin, limited sun exposure, obesity, or those living in northern regions - often reveal significant benefits, including improved bone health and other outcomes. If your blood test shows sufficient levels and you’re at low clinical risk, maintaining those levels through sensible sun exposure, a balanced diet, and modest supplementation is likely enough. High doses aren’t necessary in such cases.
Another key point is to compare the dose and duration used in studies with your own supplementation plan. For instance, if a trial used 2,000 IU daily for several years, taking 400 IU for a month won’t produce the same results. Additionally, people with obesity may require higher or adjusted doses, as standard amounts often lead to smaller increases in blood levels for them. Periodic testing and weight-adjusted dosing can help fine-tune your approach. Discussing these nuances with a healthcare provider can ensure that study findings are applied effectively to your unique needs.
By interpreting research carefully and tailoring it to your circumstances, you can make informed decisions about your vitamin D regimen. The next step is finding a supplement that matches these insights.
Using SlipsHQ to Find Quality Vitamin D Supplements
Once you’ve figured out your ideal dose, it’s time to choose a supplement that meets high standards. That’s where SlipsHQ comes in. This app bridges the gap between clinical research and the supplements on store shelves. Simply scan a product’s barcode to get detailed information, including the dose per serving (e.g., 1,000 IU, 2,000 IU, or 5,000 IU), the type of vitamin D (D2 or D3), and any added ingredients.
SlipsHQ also assigns a science-based trust score (from 0 to 100) that evaluates factors like safety, efficacy, quality, transparency, and value. This score can help you quickly identify supplements that align with evidence-based dosing, have undergone third-party purity testing, and include proper safety warnings - like caution against very high doses or potential interactions. For individuals at higher risk (such as those with darker skin, limited sun exposure, higher BMI, or osteoporosis), the app’s personalized supplement stack feature can help design a routine that fits your specific needs while staying within safe, research-backed dosing ranges.
Conclusion
Vitamin D requirements aren’t one-size-fits-all - they depend on factors like skin tone, geographic location, sun exposure, body weight, and genetics. Instead of relying on generalized findings from studies that often include participants with sufficient vitamin D levels, it’s more effective to focus on your specific risk factors and lab results. Addressing a true deficiency is crucial, but taking supplements when your levels are already adequate may not provide extra benefits and could even be harmful at very high doses.
If you’re unsure about your vitamin D levels, consider speaking with your healthcare provider about getting a 25(OH)D blood test. This is particularly important if you have darker skin, live in northern regions, spend most of your time indoors, or have a higher body mass index. With this information, you can decide whether you need a maintenance dose or a higher amount to correct a deficiency.
To make your supplementation plan more precise, leverage tools like SlipsHQ. By scanning a product’s barcode, you can instantly access details about its dosage, form, and a science-based trust score. With personalized recommendations, SlipsHQ helps you customize your vitamin D regimen to suit your individual needs - moving beyond generic advice to something that works for your unique biology.
FAQs
Why does skin tone impact vitamin D production?
Skin tone plays a role in how effectively your body produces vitamin D from sunlight. People with darker skin have higher levels of melanin, the pigment responsible for skin color. Melanin works somewhat like a natural sunscreen, limiting the skin's ability to generate vitamin D from UVB rays. As a result, individuals with darker skin often require more sun exposure to produce the same levels of vitamin D as those with lighter skin.
Why do people with obesity require more vitamin D?
People living with obesity often require more vitamin D because excess body fat tends to store the vitamin, reducing its availability for the body to use. This can result in lower levels of vitamin D circulating in the bloodstream, increasing the likelihood of a deficiency.
Research also indicates that individuals with obesity may metabolize vitamin D differently, meaning they often need higher doses to gain the same benefits as someone with less body fat. Getting enough vitamin D is crucial for maintaining overall health and supporting essential bodily functions.
Can vitamin D supplements help reduce the risk of chronic diseases?
Vitamin D supplements might help lower the risk of certain chronic illnesses, but their effectiveness can depend on several factors, including skin tone, where you live, and genetics. For instance, people with darker skin often produce less vitamin D from sunlight, and those in regions with limited sunlight may face a higher chance of deficiency.
Although vitamin D plays a key role in maintaining health - like strengthening bones and supporting the immune system - it’s not a one-size-fits-all solution for preventing every chronic condition. To figure out if supplements are a good fit for your needs, it’s always a smart move to consult a healthcare provider.